May 14, 2018Press Release
Spatial Organization of Cells in the Inner Ear Enables the Sense and Sensitivity of Hearing
Media Contact
Mass Eye and Ear Communications
communications@meei.harvard.edu
A research team from Mass. Eye and Ear has shown that the “outer hair cells” within the ear can only be effective in amplifying sound when they are configured in a Y-shaped arrangement with respect to their supporting cells.
Boston, Mass. — The loss of tiny cells in the inner ear, known as “hair cells,” is a leading cause of hearing loss, a public health problem affecting at least one out of three people over the age of 65. Of the two varieties of hair cells, the “outer hair cells” act as micromotors that amplify incoming sound, and the “inner hair cells” act to sense and transmit information about the sound to the brain. Hair cells do not regenerate on their own in human ears, and they can die away from a variety of factors including excessive noise exposure, certain medications, infection and as part of the natural aging process.
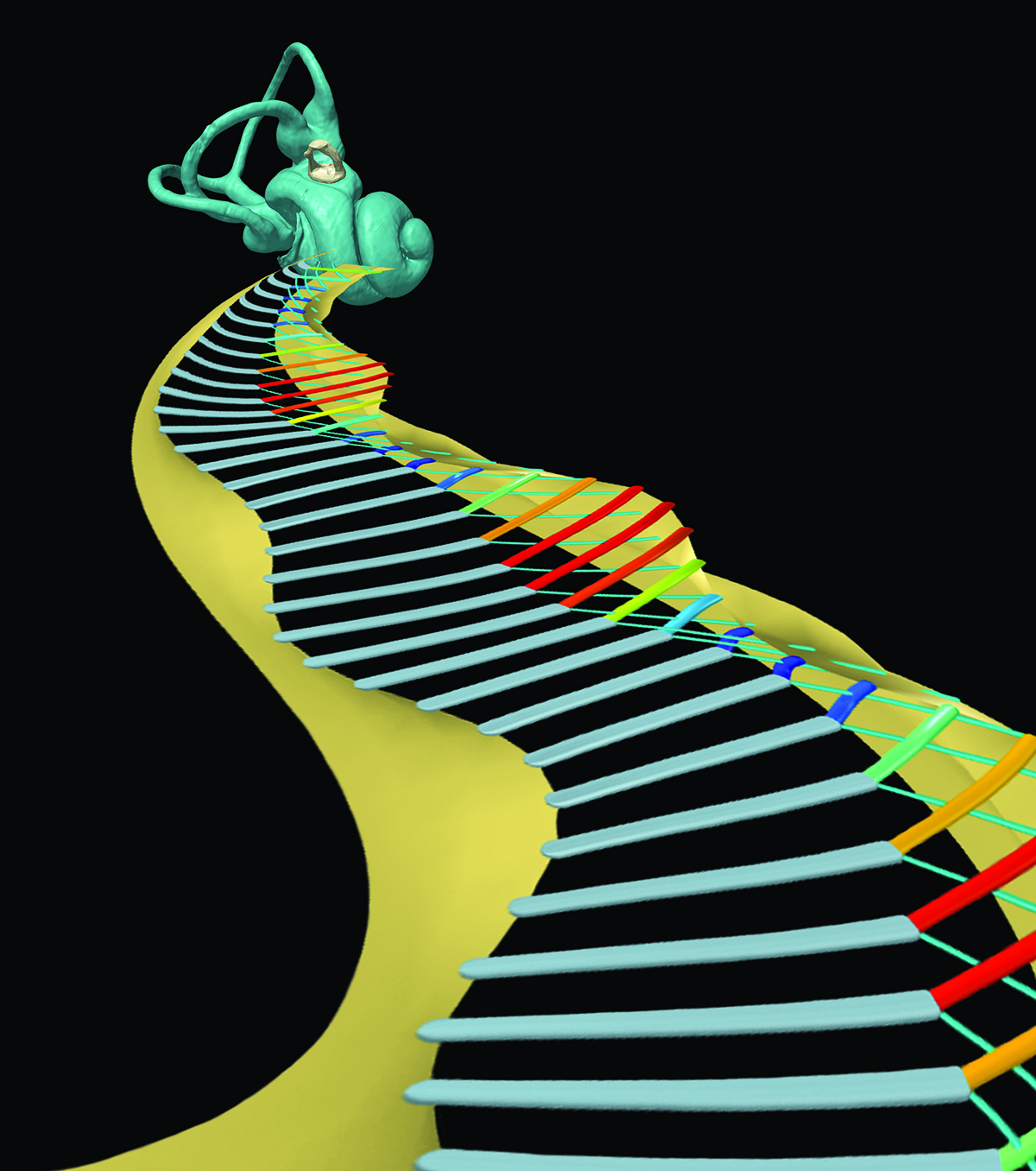 A depiction of the inner ear, with a stylized glimpse inside at the vibrating lattice of ‘Y-shaped’ cellular architecture found within the organ of Corti. Image courtesy of Hamid Motallebzadeh, Garyfallia Pagonis, Peter Gottlieb, Haobing Wang, and Sunil Puria.
A depiction of the inner ear, with a stylized glimpse inside at the vibrating lattice of ‘Y-shaped’ cellular architecture found within the organ of Corti. Image courtesy of Hamid Motallebzadeh, Garyfallia Pagonis, Peter Gottlieb, Haobing Wang, and Sunil Puria.
Researchers around the world are working to restore human hearing by regenerating outer hair cells in the cochlea of the inner ear, the loss of which is a leading cause of hearing impairment, through a variety of techniques, and some have even shown success in restoring some hearing sensitivity in animal studies. However, new research shows that restoring hearing is not just about regenerating the lost outer hair cells. In a study published online today in the journal Proceedings of the National Academy of Sciences (PNAS), a research team from Mass. Eye and Ear has shown that, in order to effectively amplify and tune sound, each of the outer hair cells must be arranged as a specific branch of a Y-shaped building block, which is replicated thousands of times within the cochlea to form a highly organized cellular architecture.
“Our work suggests that, in order for humans to hear well, the outer hair cells in the cochlea not only need to be in good working order, but also need to be connected to other nearby cochlear structures in a very particular way,” said senior author Sunil Puria, Ph.D., an Amelia Peabody Scientist at Mass. Eye and Ear and instructor in otolaryngology at Harvard Medical School. “It had been assumed that, if we could just succeed in regenerating outer hair cells, it would be sufficient to restore hearing. But our work shows that the spatial organization of the restored cells must also be taken into account.”
Motivated by previous studies in their lab, the researchers created a detailed computer simulation of the cochlea and the tiny structures within it. They then tested how different arrangements and malformations of the Y-shaped structures affect hearing function. They found that the outer hair cells could only produce high hearing sensitivity and frequency selectivity when arranged in their natural configuration with respect to the surrounding structures. When they altered the geometry and material properties of these structures, the cells’ ability to amplify and tune sound was compromised.
The study provides an important step toward understanding the functional implications of how the outer hair cells are arranged in the inner ear – with far-reaching implications for emerging new clinical therapies that aim to restore hearing by regenerating these cells, but not necessarily in a way that restores their critical position within the natural Y-shaped building blocks of the cochlea.
“We built our model to test whether rearranging the cells in the Y-shaped structures of the inner ear alters the ear’s ability to amplify sound,” said Dr. Puria. “By altering these structures in the model, we see strong evidence that amplification and tuning in the cochlea depend heavily on the natural arrangement of these structures.”
According to co-author Hamid Motallebzadeh, Ph.D., a postdoctoral fellow at Mass. Eye and Ear/Harvard Medical School, “Computational models such as the one developed for this study can be used to replicate and interpret experimental measurements, thus potentially reducing the need for animal-based studies, and can also allow researchers to conduct well-controlled ‘virtual experiments’ that go far beyond what is currently possible to perform in actual experiments.”
The authors on the PNAS paper include Dr. Motallebzadeh, Dr. Puria and Dr. Joris A. M. Soons, of the University of Antwerp.
This research was supported in part by National Institute on Deafness and Other Communications Disorders grant R01 DC07910.
About Massachusetts Eye and Ear
Massachusetts Eye and Ear, founded in 1824, is an international center for treatment and research and a teaching hospital of Harvard Medical School. Specializing in ophthalmology (eye care) and otolaryngology-head and neck surgery (ear, nose and throat care), Mass. Eye and Ear clinicians provide care ranging from the routine to the very complex. Also home to the world's largest community of hearing and vision researchers, Mass. Eye and Ear has pioneered new treatments for blindness, deafness and diseases of the head and neck. Our scientists are driven by a mission to discover the basic biology underlying these conditions and to develop new treatments and cures. In the 2017-2018 "Best Hospitals Survey," U.S. News & World Report ranked Mass. Eye and Ear #1 in New England for eye (#4 in nation) and ear, nose and throat care (#2 in nation). For more information about life-changing care and research at Mass. Eye and Ear, please visit our blog, Focus, and follow us on Twitter and Facebook.

